OUR SERVICES
Innovative tech-driven solutions for optimized revenue cycle management.
Viorcm Healthcare Revenue Cycle Management Solutions
VIORCM provides comprehensive Revenue Cycle Management (RCM) services, designed to significantly enhance efficiency, optimize financial performance, and streamline business processes for healthcare providers.
Provider Credentialing & Enrollment:
Documentation: Collection, validation, and secure storage of essential credentialing documents.
Payer Submission: Timely submission of accurate applications to major payers according to their specific formats.
Ensure Enrollment: Continuous follow-up and verification to confirm successful enrollment.
Updates & Re-Credentialing: Regular management and updating of documents to ensure continuous payer credentialing compliance.
Eligibility & Benefits Verification and Prior Authorization:
Proactive verification to prevent delays, reduce rework, and enhance patient satisfaction.
Expert initiation and follow-up on prior authorization requests via payer portals and direct communications.
Patient Demographics:
Accurate registration of patient details and precise selection of insurance codes.
Effective data management to ensure clean claims, minimizing denials and rejections.
Medical Coding & Claim Scrubbing:
AAPC and AHIMA-certified coding specialists proficient in diverse medical specialties.
Accurate assignment of ICD-10, CPT, HCPCS codes, and modifiers.
Comprehensive claim scrubbing, focusing on:
Patient information verification (name, DOB, insurance details)
Correct coding validation for accuracy and service matching
Compliance with payer-specific guidelines
Duplicate claim prevention
Enhanced reimbursement rates through meticulous claim reviews prior to submission.
Charge Entry & Claim Submission:
Efficient processing of both manual and electronic charge entries sourced from EHR/EMR systems.
Accurate and timely claim submissions for prompt payer response.
Payment & Denial Posting:
Payments from ERA/EOB are posted promptly (within 24-48 hours).
Daily reconciliation reports.
Immediate forwarding of denials to the dedicated denial analysis team.
Denial & Rejection Management:
Thorough analysis to identify root causes of claim denials.
Proactive corrective actions to address and resolve recurring denial issues.
Weekly comprehensive denial analysis reports provided to clients.
Accounts Receivable (AR) Management & Follow-Up:
Effective AR strategies to reduce outstanding receivables and accelerate cash flow.
Identification and proactive management of underpayments, enhancing overall profitability.
Patient AR & Collections:
Systematic management of outstanding patient balances due to unpaid co-pays, deductibles, coinsurance, or self-pay scenarios.
Structured patient collections processes:
Initial patient billing and invoicing.
Follow-up communications and timely reminders.
Flexible installment payment plan options.
Collaboration with reputable third-party collection agencies when necessary.
Legal actions reserved for exceptional cases.
VIORCM ensures diligent management of patient AR and collections, maintaining consistent revenue streams and financial stability for healthcare providers.
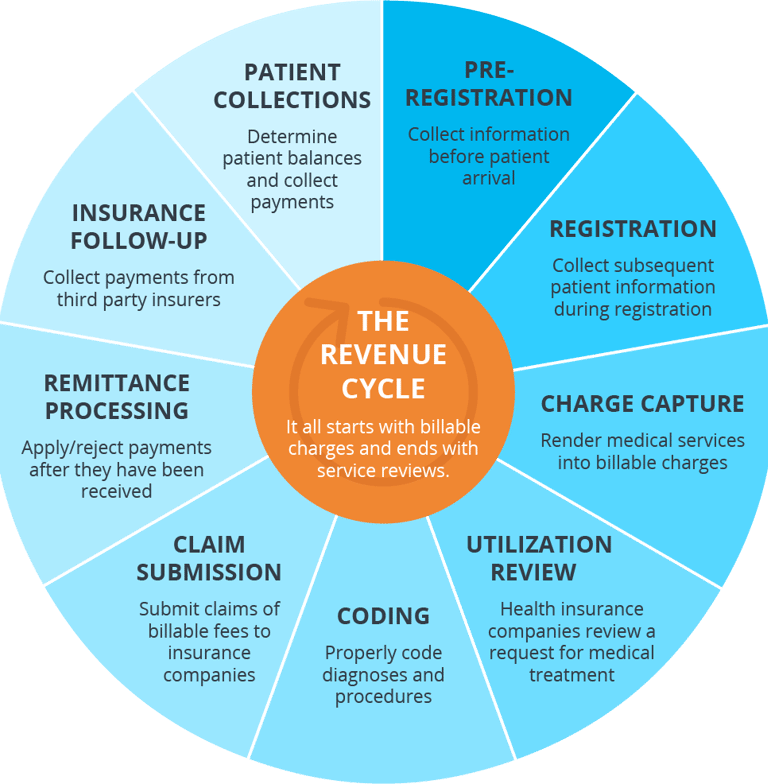

Viorcm- End-to-End RCM Solutions
Solutions
Expertise in revenue cycle management for healthcare.
Success
info@viorcm.com
+1 302 231 1259
© 2025. All rights reserved.
